If you have diastolic heart failure, your heart’s left ventricle becomes thick and stiff. As a result, it doesn’t fill with enough blood between beats. Since there’s less blood in the ventricle, your heart can’t pump out enough to meet your body’s needs. Doctors also call it heart failure with preserved ejection fraction, or HFpEF. Since it sticks around long-term, we call it “chronic”—which means it needs ongoing care and lifestyle changes to stay under control.
Now, compare that with systolic heart failure, where the heart can’t pump strongly enough. One deals with stiffness, the other with weakness. So even though both are types of heart failure, they work differently and need different treatments. Knowing the difference helps you understand what’s going on and how to manage it better.
Causes and Risk Factors of Chronic Diastolic Heart Failure
Understanding the causes of chronic diastolic heart failure can help you take early steps to protect your heart. Let’s look at the most common reasons and risk factors that lead to this condition.
1. High Blood Pressure (Hypertension)
High blood pressure is one of the most common causes of chronic diastolic heart failure. It forces the heart to pump harder, which thickens and stiffens the heart walls. Over time, this makes it difficult for the heart to relax and fill properly between beats.
2. Diabetes
Diabetes affects the heart by damaging blood vessels and changing how the heart muscle works. When blood sugar stays high, the heart becomes less flexible. This stiffness raises the risk of heart failure, especially if diabetes is not well managed.
3. Aging and Natural Heart Stiffness
As people age, their heart muscles slowly lose flexibility. This change is natural, but it makes it harder for the heart to relax after each beat. Because of this, older adults face a higher risk of developing diastolic heart failure.
4. Other Medical Conditions
Several health issues contribute to heart stiffness and poor function. These include obesity, kidney disease, coronary artery disease, and sleep apnea. Each of these conditions puts extra pressure on the heart and increases the chances of heart failure over time.
5. Genetic and Family History
Some people inherit heart traits that make them more prone to diastolic heart failure. Even if you live a healthy life, your genes can still affect how your heart functions. That’s why it’s important to know your family’s heart health history.
6. Lifestyle Factors
Daily habits play a big role in heart health. Smoking, eating unhealthy foods, skipping exercise, and drinking too much alcohol all strain the heart. Over time, these habits can lead to the causes of chronic diastolic heart failure and raise overall risk.
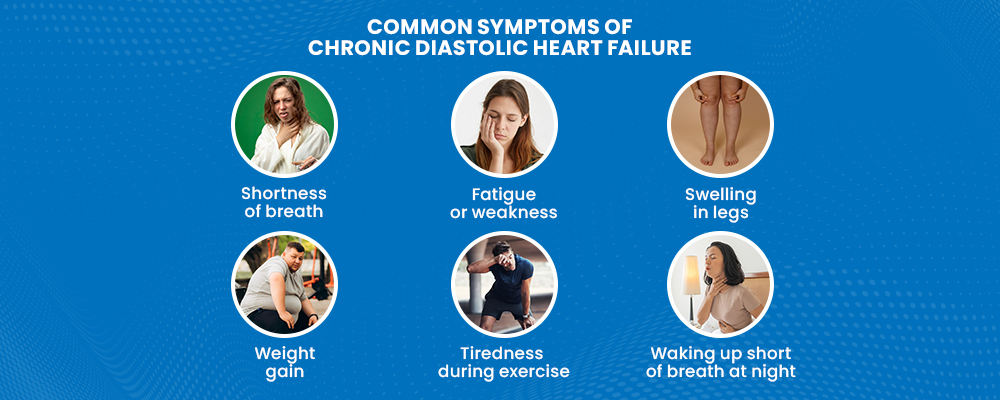
Signs and Symptoms of Chronic Diastolic Heart Failure
The symptoms of chronic diastolic heart failure may appear gradually. Paying attention to these signs can help with early diagnosis and better management.
Common symptoms include:
- Shortness of breath
You may feel breathless during activity, rest, or while lying flat due to fluid buildup in the lungs. - Fatigue or weakness
The heart struggles to meet your body’s energy needs, making you feel unusually tired, even after mild activity. - Swelling in legs, ankles, or abdomen
Poor circulation causes fluid retention, leading to noticeable puffiness or bloating in these areas. - Weight gain from fluid buildup
Sudden or steady weight gain may signal the body is holding onto extra fluid. - Reduced ability to exercise
Simple tasks may feel difficult or tiring, especially as the condition progresses. - Waking up short of breath at night
This is a sign fluid is affecting your breathing when you lie down. - Trouble concentrating or memory issues
Less blood flow to the brain may lead to confusion or forgetfulness.
How Is Chronic Diastolic Heart Failure Diagnosed?
Diagnosing chronic diastolic heart failure involves a mix of physical exams, blood tests, and heart imaging. Since symptoms often overlap with other conditions, your doctor needs a clear picture of how your heart is functioning.
1. Physical Exam and Medical History
It starts with your doctor listening to your symptoms and asking about your medical history. They’ll check for signs like swelling, irregular heartbeat, or lung congestion. Sharing a complete history helps your doctor connect the dots faster.
2. Echocardiogram
This is the key test for spotting diastolic heart failure. An echocardiogram uses sound waves to show how well your heart moves and pumps. In diastolic heart failure, the heart’s pumping strength—called ejection fraction—is usually preserved. But the heart has trouble relaxing and filling with blood properly. That’s the main clue doctors look for.
3. Exercise Stress Test
An exercise stress test shows how your heart performs under physical stress, typically while walking on a treadmill. It helps doctors detect issues with blood flow, heart rhythm, or other cardiac functions during increased activity.
4. Imaging and Other Tests
Sometimes, additional tests like a chest X-ray, ECG, or MRI are needed. These help rule out other causes and give more details about your heart and lungs. Your doctor may also check kidney function or look for signs of other related conditions.
Treatment Options for Chronic Diastolic Heart Failure
Managing chronic diastolic heart failure involves a mix of lifestyle changes, medications, and regular medical care. The goal is to ease symptoms, improve heart function, and prevent complications.
1. Lifestyle Changes
Making healthy changes in your daily routine plays a big role. Doctors recommend eating a heart-friendly diet low in sodium, staying active with regular exercise, and avoiding smoking or excessive alcohol. These habits reduce the heart’s workload and help control symptoms.
2. Medications
Your doctor may prescribe medicines to help your heart work better. Diuretics help remove extra fluid and reduce swelling. Beta-blockers and ACE inhibitors control blood pressure and protect the heart. Taking medicines as prescribed can improve your quality of life.
3. Managing Underlying Conditions
Treating related health problems like high blood pressure or diabetes is essential. Controlling these conditions prevents further heart damage and supports better overall health. Regular check-ups help keep these conditions in check.
4. Monitoring and Regular Follow-ups
Keeping in touch with your healthcare team is key. Regular follow-ups let doctors track your progress, adjust treatments, and catch any problems early. Monitoring your symptoms and reporting changes promptly helps you stay on the right path.
Moreover, for individuals seeking advanced options, heart failure clinical trials provide access to potential new treatments not yet widely available. Participation also helps advance research while ensuring expert care and close monitoring.
Frequently Asked Questions
1. How long can you live with diastolic dysfunction?
If you have diastolic dysfunction without coronary artery disease, your lifespan is usually similar to others your age. However, the outlook is somewhat less favorable if you also have other heart conditions, such as coronary artery disease or systolic heart failure.
2. What are the best exercises for heart failure?
- Gentle brisk walking, using a walking stick if needed.
- Light jogging, once you’ve built up strength through walking.
- Cycling on flat, easy routes.
- Swimming and water aerobics.
- Mindful breathing exercises such as Tai Chi, Baduanjin, Liuzijue, and Wuqinxi.
What should you avoid if you have diastolic dysfunction?
Maintain a healthy weight and avoid tobacco while limiting alcohol and caffeine. Eat a balanced diet with plenty of fruits, vegetables, whole grains, healthy fats, and lean protein. Aim for at least 150 minutes of aerobic exercise weekly. Follow your healthcare provider’s advice, manage stress through meditation or therapy, limit unhealthy fats, sodium, and sugar, and get 7–8 hours of sleep each night.
Conclusion:
In conclusion, chronic diastolic heart failure requires ongoing care and lifestyle changes to manage symptoms and improve quality of life. Early diagnosis, proper treatment, and strong support systems play key roles. Staying informed and proactive empowers patients and caregivers to navigate this journey with hope and confidence.




