Systemic Lupus Erythematosus (SLE) is a long-term illness where the body’s immune system becomes overactive and starts attacking its own healthy tissues and organs. It is a type of autoimmune disorder that can affect different parts of the body at the same time.
Let’s break it down in simple terms so you can easily understand what it is, how it affects the body, and what can be done to manage it.
What is Systemic Lupus Erythematosus (SLE)?
Your immune system is supposed to protect you from germs and infections. But in Systemic Lupus Erythematosus, the immune system gets confused and instead of protecting, it starts attacking your own body. As a result, this immune dysfunction causes widespread inflammation that affects the skin, joints, kidneys, brain, blood cells, and other internal systems.
Unlike localized autoimmune conditions, SLE is “systemic,” meaning it affects multiple systems simultaneously or in cycles. It often flares up unpredictably, with periods of worsening symptoms, and then gets better for a while before coming back again.
Types of Lupus
Doctors often use the term Systemic Lupus Erythematosus (SLE) when talking about lupus because it can affect many parts of the body. But lupus is not just one disease—there are different types, and each one affects the body in its own way.
To better understand these types and find new, more effective treatments, Clinical Trials for SLE are currently being done. These trials help researchers create medicines that are more targeted and helpful for people with lupus.
Following are the main types of lupus:
1. Cutaneous Lupus
Cutaneous lupus mainly affects the skin. It can cause rashes, sores, and hair loss. The most well-known rash that appears in cutaneous lupus is the butterfly rash. It is a red, scaly rash that appears across the cheeks and the bridge of the nose. Additionally, this type of rash is sensitive to sunlight and sometimes causes permanent scarring as well.
2. Drug-Induced Lupus
Certain medications that are used to treat other health problems, such as high blood pressure or infections, can trigger SLE-like symptoms as a side effect. However, this type of lupus is usually temporary and might go away after you stop taking the medication that caused it.
3. Neonatal Lupus
It is a rare condition that happens in newborn babies. Although it’s not true lupus but it can be caused by certain antibodies passed from the mother during pregnancy. Therefore, babies with neonatal lupus may have skin rashes, liver problems, or low blood cell counts. But most symptoms go away within a few months.
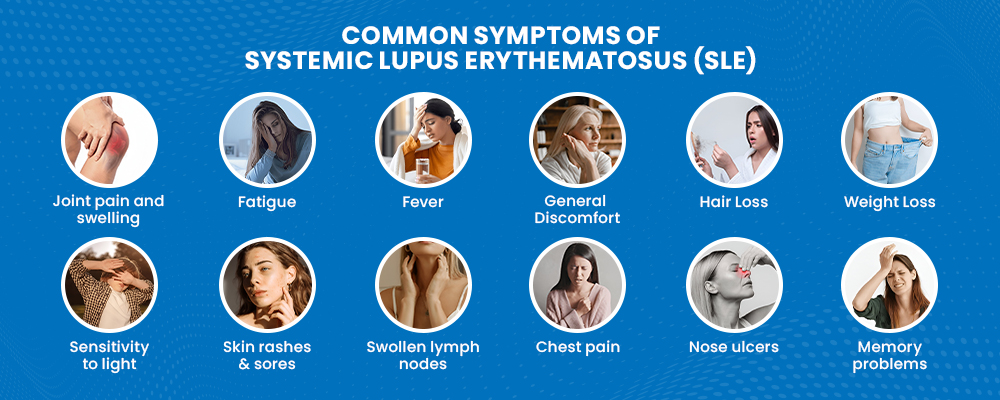
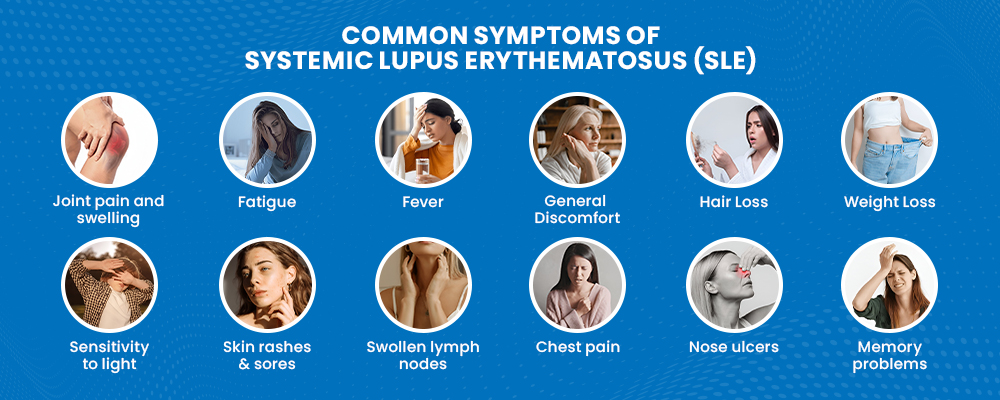
Symptoms of Systemic Lupus Erythematosus
Symptoms vary from person to person and may come and go. These are called flares (when symptoms get worse) and remission (when symptoms improve or go away for a while). The most common symptoms of SLE are as follows:
- Joint pain and swelling (especially in fingers, wrists, and knees)
- Fatigue
- Fever without any cause
- General discomfort or uneasiness (malaise).
- Hair loss
- Weight loss
- Sensitivity to light
- Skin rashes and sores
- Swollen lymph nodes
- Chest pain while breathing deeply
- Mouth or nose ulcers
- Memory problems or confusion
Moreover, some other symptoms might also appear, depending on which part of the body is affected:
- Brain: Headaches, numbness, tingling, memory issues, seizures, or personality changes
- Stomach: Abdominal pain, nausea, vomiting
- Heart: Valve problems or inflammation of heart muscles and pericardium.
- Lungs: Chest pain, trouble breathing, coughing up blood (especially when breathing deeply)
- Skin: Mouth sores, rashes
- Kidneys: Swelling in the legs, lupus nephritis
- Blood Vessels: Clots, vessel inflammation, cold fingers/toes (Raynaud’s Phenomenon)
- Blood Cells: Low red cell count (Anemia) as well as low white cell and platelet count.
Do you know?
Despite having lupus, some people only develop skin symptoms. This is called discoid lupus.
What Causes Systemic Lupus Erythematosus?
Doctors are not exactly sure what specifically causes SLE. However, some factors can make it more likely to get. These include:
1. Family History (Genes):
If lupus runs in your family, you may be more likely to develop it. That is because certain genes can make your immune system more sensitive to disease.
2. Hormones:
SLE is more common in women than men by nearly 10 to 1. It may occur at any age. However, it appears most often in young women between the ages of 15 and 44. It may be linked to female hormones like estrogen, which might affect how the immune system works.
3. Infections and Viruses:
Infections like the Epstein-Barr virus (which causes mono) can sometimes trigger lupus, especially in people who already have a higher risk.
4. Sunlight (UV Exposure):
Spending too much time in the sun can trigger lupus symptoms or cause skin rashes, especially in people with cutaneous lupus or photosensitivity.
5. Certain Medications:
Some medicines, like those used for blood pressure, heart disease, or infections, can certainly cause drug-induced lupus.
6. Physical or Emotional Stress:
Major stress, such as surgery, serious injury, or emotional trauma, may trigger or worsen lupus symptoms in some people.
How is SLE Diagnosed?
Lupus can be tricky to diagnose because its symptoms are similar to many other illnesses. Therefore, the American and European Rheumatology societies have published classification criteria to assist in the diagnosis of SLE. It includes the following approaches:
1. Medical History
The doctor will begin by asking about your symptoms and how long you’ve been experiencing them. In addition, the doctor may ask whether anyone in your family has lupus or similar autoimmune diseases, because it increases your risk.
2. Physical Exam
During the physical exam, the doctor will check your joints for swelling or pain. They will also examine your skin for any rashes or mouth sores. Moreover, the doctor may also check other parts of your body for signs of inflammation.
3. Blood Tests
Your healthcare provider might order some blood tests to help check for signs of lupus and rule out other conditions. These tests include:
- ANA (Antinuclear Antibody): Most people with lupus have a positive ANA test.
- Anti-dsDNA and Anti-Smith Antibodies: These are more specific to lupus and help confirm the diagnosis.
- CBC (Complete Blood Count): Checks for anemia, low white cells, or low platelets.
- ESR and CRP: Show if there’s inflammation in your body.
- RFT: To detect any damage caused to the kidneys.
- LFT: To check whether the liver is working fine.
4. Urinalysis
Urine tests can be done to look for blood or protein in your urine, which can be a sign that lupus is affecting your kidneys.
5. Imaging or Biopsy
Imaging tests like chest X-rays or echocardiograms may be done if your lungs or heart are affected. Also, a biopsy of the skin or kidney (taking a small sample of tissue) can be done to check for damage caused by lupus.
Treatment for Systemic Lupus Erythematosus (SLE)
There is no definite cure for SLE, but it can be managed through treatments that help control the symptoms and prevent further complications. However, every person with SLE is different, so doctors choose the treatment based on several factors, including:
- How active is the disease?
- Which organs or body parts are affected?
- Which treatment options are the safest and most effective for that individual?
Treatment for Mild SLE
If your lupus is mild, your doctor may suggest:
- NSAIDs (Nonsteroidal Anti-Inflammatory Drugs): These can help with joint pain and chest pain from the pleurisy. However, always talk to your doctor before using them.
- Low-dose corticosteroids (e.g., prednisone): These help to reduce inflammation in the skin and joints.
- Corticosteroid creams: These are used directly on skin rashes to reduce redness and itching.
- Hydroxychloroquine: Even though it is an anti-malarial drug, it is also used to treat lupus and helps prevent flare-ups.
- Methotrexate: This can be used to help reduce the need for steroids.
- Biologic medicines (belimumab, rituximab, and anifrolumab): All these newer drugs may help some people by targeting the immune system more directly.
Treatment for Severe SLE
If lupus affects major organs and becomes more serious, then stronger treatment is needed. This may include:
- High-dose corticosteroids: These help to quickly reduce serious inflammation.
- Immunosuppressive drugs: These medicines calm down the immune system. They are used if lupus is affecting the brain, kidneys, or other important organs, or if steroids alone are not working. Some common medicines include:
- Voclosporin
- Azathioprine
- Mycophenolate
- Rituximab (sometimes used in certain cases)
- Cyclophosphamide (used only for short periods because of side effects)
- Blood thinners (i.e., warfarin): These are used if you have blood-clotting problems, such as antiphospholipid syndrome.
Other Important Tips for Living with Lupus
In addition to treatments, it is also important to follow these tips:
- Wear protective clothing, sunglasses, and sunscreen when in the sun.
- Take preventive heart care by getting regular checkups and managing your blood pressure and cholesterol levels.
- Stay up-to-date on vaccines because they help prevent infections.
- Talk to your doctor and get a bone scan. This is because lupus and steroid use can lead to bone thinning (osteoporosis). Hence, screening is important.
- Avoid smoking and limit alcohol because these can make lupus worse and affect your overall health.
Outlook (Prognosis)
The outcome for people with Systemic Lupus Erythematosus (SLE) has improved a lot in recent years. Many people now experience only mild symptoms, especially with proper treatment. However, how well a person does depend on how severe their lupus is and which parts of the body are affected.
Most people with SLE will need to take medicine for a long time. Hydroxychloroquine is commonly prescribed and is often taken for life to help control the disease.
Even though treatments have improved, SLE is still a serious condition. In the United States, it is one of the top 20 leading causes of death among females aged 5 to 64 years. This is because lupus tends to be more active:
- In the first few years after diagnosis
- In people under the age of 40
So, in order to help improve outcomes, Systemic Lupus Erythematosus Clinical Trials are being conducted. These research studies test new and better treatments for lupus, giving hope for more effective and safer options in the future.
Conclusion
Systemic Lupus Erythematosus (SLE) is a complex autoimmune disease that can affect many parts of the body and impact daily life in serious ways. Although there is currently no cure, advances in medical care and ongoing research have greatly improved the outlook for people living with this condition. With the right treatment plan, most people with lupus can manage their symptoms and lead fulfilling lives.
Moreover, clinical trials such as those conducted by Hightower Clinical offer hope for newer and more effective lupus treatments. Thus, by staying informed and participating in ongoing studies, patients can make a big difference in managing lupus long-term.
Remember: Lupus may be lifelong, but with proper care, support, and awareness, it doesn’t have to define your life.




